Mention Goodman and Gilman to any pharmacologist, and they will automatically think of their graduate school textbook. Generations of pharmacologists have indelibly linked the duo as naturally as Mercedes-Benz and Baskin-Robbins. Actually, Louis Goodman and Alfred Gilman carved distinctly separate career paths, except for two key activities. We can be grateful that their two joint ventures were major contributions to pharmacology and experimental therapeutics.
The Textbook
Alfred Gilman was born in 1908 in Bridgeport, Conn., the son of a music store owner.1,2 He received his undergraduate and graduate education at Yale University, earning a PhD in physiological chemistry in 1931.1,3,4 Gilman stayed at Yale as a postdoctoral fellow in pharmacology and then joined the faculty in 1932, with eight published papers already to his credit. He was slender, and in those days, played tennis and squash. He also enjoyed sailing and fishing.2
Gilman was generous and quick to praise his colleagues. Years later, as a senior researcher, he would cut his modest office in half to make room for a junior faculty member. He eventually closed his lab when he decided another member of the department could make better use of the space.1
Louis S. Goodman (the one with the mustache) was born in 1906 in Portland, Ore., the son of an optometrist. He graduated from Reed College, earned his MD from the University of Oregon in 1932, and then served his internship at Johns Hopkins Hospital.2,5,6 Goodman’s first publications were chapters that he was invited to write for medical textbooks. He was somewhat taller and heavier than Gilman, and his idea of exercise was picking up and reading a book or journal.2
Goodman had a keen wit, was sometimes gruff and held strong opinions. His often-colorful quips earned him the nickname, Louie the Lewd.1,6 He constantly coaxed and cajoled everyone to work harder. One colleague said, “If you didn’t do well, you heard about it.”5
The pair met in 1934, when Goodman was awarded a fellowship by the National Research Council to conduct research in the pharmacology department at Yale. Lackluster medical student attendance in the pharmacology course (due to poor quality lectures) prompted Milton Winternitz, Dean of the Medical School, to ask Goodman and Gilman to run the course.2 Even as assistant professors, they were recognized as excellent lecturers.
They found both of the available pharmacology textbooks unsatisfactory. One was unreadable, and the other was out of date.2,4 Instead, they compiled their lecture notes largely from contemporary journal articles and combined basic pharmacology, physiology and biochemistry with clinical medicine.5
Goodman had always been interested in pharmacology, read widely and remembered everything he read.2 By all accounts, he was also an excellent writer. Having written book chapters and monographs, he thought he could write a much better pharmacology textbook, especially if he had help from Gilman. Gilman was less eager and probably would not have considered writing a textbook on his own.2,5
Goodman drafted the first few chapters and sent them to colleagues for feedback. They not only encouraged him but also alerted a publisher, Macmillan Company.4,5 When Macmillan presented the two lecturers with a publishing contract in 1938, Gilman enthusiastically joined Goodman as a full partner in the work.2,5
They wrote every chapter themselves. Mirroring their lectures, the book described pharmacology in the context of clinical therapeutics, a novel approach at the time.6,7
Macmillan wanted a 450,000-word textbook, but Goodman and Gilman submitted a manuscript of nearly 1,000,000 words.2,4,6 The publisher balked because comparable textbooks were never that lengthy or expensive. The authors held firm, saying “take it or leave it.”4
Macmillan printed 3,000 copies and agreed to publish a second edition, if the book sold out within four years. Gilman confidently bet a case of Teacher’s Highland Cream whisky that the high-priced, four-pound textbook would reach that goal.2,5,6
The first edition of The Pharmacological Basis of Therapeutics was published on January 7, 1941. Just six weeks later, Goodman and Gilman received their case of scotch.2,5 In total, about 115,000 copies were sold.2
As a footnote to this achievement, Gilman’s son was born six months later, on July 1, 1941, and was named Alfred Goodman Gilman, in honor of Gilman’s good friend. Years later, the younger Gilman was chided by classmates, who proclaimed that he was the only person ever named for a textbook.1
World War I Gases
Although Milton Winternitz retired as dean in 1935, he remained at Yale. World War II was raging in Europe and would soon involve the United States. Of great concern was the potential use of chemical weapons, and Winternitz was chairman of the Committee on the Treatment of War Gas Casualties, a group of respected academic scientists who were advising the government. Winternitz had written and edited sections of the definitive monograph on pathology of war gases and was generally regarded as the most prominent expert in the field.8
Modern chemical warfare began on April 22, 1915, when the German army used chlorine gas for the first time in large-scale offensive action.8–11 Subsequently, both sides in World War I developed chemical weapons, including phosgene and Lewisite.9
On July 12, 1917, German forces first used mustard gas against the British at Ypres, Belgium.9–14 Within a year, the Allies were also deploying mustard gas, and both sides soon realized that the best way to deliver the gas was in artillery shells.10
Victor Meyer first prepared dichloroethyl sulfide in 1886.12,13,15 The yellow-brown chemical had a very characteristic odor suggestive of garlic or mustard, hence its common name.10,13,15
Mustard gas is actually an oily liquid at room temperature. When exploded via bombs over enemy troops and trenches, it dispersed as an aerosol. The aerosol stuck to skin, clothing and surfaces, and could pass through leather, rubber and most textiles. It could also persist on the contaminated ground for weeks.9,10
Mustard gas caused no immediate effects. Consequently, troops marched through contaminated areas unaware that they were being exposed. About 12 hours later, their skin, eyes and mucous membranes became irritated.9–11,13
The extreme eye irritation felt like gritty sand, and some troops were temporarily blinded. Exposed skin developed large, painful blisters and ulcers. Without quick washing, the ulcers festered. The inhaled aerosol caused respiratory distress, pulmonary edema and damage to the bronchial tubes.9,10
There was no antidote, and victims were incapacitated for weeks, sometimes months. Those who received prompt and diligent nursing care generally recovered. The fatality rate was just 2–3%. But because of the slow recovery, mustard gas severely diminished the army’s ability to fight.10,13
The effectiveness of mustard gas made it the chemical weapon of choice from 1917 onward.8,13 It accounted for nearly 400,000 casualties, more than any other chemical weapon.10,13
But by the end of World War I, researchers had devised clothing and masks that offered adequate protection.9

Between the Wars
Funding for chemical weapon research, understandably, was greatly reduced following the war.16,17 The work and researchers were consolidated at Edgewood Arsenal in Maryland under the U.S. Army’s Chemical Warfare Service.8,10,13
Edward Krumbhaar, a captain in the U.S. Army Medical Corps, studied victims who survived mustard gas intoxication and saw that they suffered a profound loss of white blood cells.11,12 His findings, which were published in 1919, were the first clinical report of this effect. In the 1920s, a few other researchers reported sulfur mustard’s effect on blood-forming tissues.16
During this time, chemists developed nitrogen-substituted analogs of sulfur mustard. In 1931, clinicians at New York’s Memorial Hospital successfully treated 13 patients by applying nitrogen mustard directly to superficial skin cancer.17
No investigator delivered the mustard agents systemically for any type of cancer, and these few isolated reports went largely unnoticed.16,18
Reviving Research
At the dawn of World War II, the Chemical Warfare Service was revitalized to investigate, develop, manufacture, and supply both chemical weapons and protective anti-gas equipment. The U.S. and its Allies did not intend to use chemical weapons, but they maintained stockpiles as a precaution and to retaliate in case they were attacked with chemical agents.8,11,13
A young military physician, Stewart Alexander, took over as director of the Medical Division at the Chemical Warfare Service. His large laboratory group conducted secret research on the chemical agents’ toxicity and ointments that might protect against skin blistering.8,11,13
In April 1942, Alexander began a two-month series of experiments to study nitrogen mustard. The effects on the skin, eyes and lungs of rabbits were similar to the well-known effects of sulfur mustard used in World War I.8
Alexander also coordinated the military’s research contracts on behalf of the National Defense Research Committee. About two dozen contracts were awarded to academic researchers around the country. Those researchers conducted a wide range of secret experiments on chemical weapons and possible antidotes. The Committee on the Treatment of War Gas Casualties assisted with administering and supervising the contracts.8,13
Early in 1942, Winternitz, chairman of the Committee on the Treatment of War Gas Casualties, brokered a military contract for Yale. He assigned Goodman and Gilman to study sulfur and nitrogen mustards.
The Yale Contract
Early in 1942, Winternitz, chairman of the Committee on the Treatment of War Gas Casualties, brokered a military contract for Yale.11,13,18,19 He assigned Goodman and Gilman to study sulfur and nitrogen mustards.19
The Yale researchers maintained close communications with the other groups holding classified military contracts. They shared their results and met frequently. This permitted the researchers to rapidly elucidate the mustard agents’ “unique and fascinating properties.”19
When given systemically, the sulfur and nitrogen mustards produced a wide range of pharmacological effects on cells, tissues, and enzymes.16 At “threshold doses” (that is, the lowest dose that produced an effect), the compounds damaged only cells and tissues with high rates of growth and proliferation: blood cells, blood-forming organs (bone marrow and lymphatic tissue), and the mucosa of the gastrointestinal tract. The damage to circulating white blood cells (lymphocytes and granulocytes) was rapid and dose-dependent.16,19
They could not elucidate the molecular mechanism of action, but they did make one insightful observation. The mustards produced “profound disturbances” on the structure and function of fruit fly chromosomes.16
Goodman and Gilman focused their studies on the pharmacological actions and toxicity of mustard agents, primarily in rabbits.13,19 They showed that toxicity was due to the mustards’ extreme chemical reactivity. Sulfur mustard forms a highly reactive sulfonium ion, and the nitrogen mustards form a reactive imonium ion.9,16,20
We now know that these reactive ions alkylate DNA, forming covalent bonds that prevent cell proliferation. The reactive ions can also alkylate any other tissues, proteins and biochemicals that they contact.12
The mustards’ actions were unlike any other chemical compound, but the effects resembled X-ray exposure.16,17,21
Goodman and Gilman also conducted experiments aimed at finding an effective antidote. To evaluate the efficacy of each potential antidote, they measured its ability to protect against the decrease in white blood cell counts, which was the most sensitive measure of mustard toxicity.16
They found that thiosulfate pretreatment seemed to protect rabbits the best. This suggested that thiosulfate could be an effective antidote, at least under ideal laboratory conditions.19
In parallel, Stewart Alexander’s group at Edgewood Arsenal also observed that systemically administered nitrogen mustard caused deterioration of lymph nodes and bone marrow in rabbits, as well as a severe decrease in white blood cell counts. They saw the same effects in various animals. On June 30, 1942, Alexander described his results in a classified memorandum, which was shared with Yale and the other research groups.8
Goodman and Gilman focused their studies on the pharmacological actions and toxicity of mustard agents, primarily in rabbits. They showed that toxicity was due to the mustards’ extreme chemical reactivity.
Mouse Lymphoma
The remarkable sensitivity and vulnerability of rapidly proliferating cells and lymphoid tissues suggested that the mustards might effectively treat lymphoid tumors. Goodman and Gilman showed their rabbit data to Thomas Dougherty, a Yale anatomy professor, and he agreed to assist with the first efficacy studies.16,19
Sulfur mustard had undesirable physical properties for these studies.16 It was volatile, quite insoluble, unstable in water, dangerous to handle and difficult to administer.17
The nitrogen mustard analogs were slightly less reactive than sulfur mustard.16,21 They formed non-volatile, water-soluble hydrochloride salts, could be handled safely, and could be administered intravenously.16,17
In the first series of experiments, they injected mice to determine the acute lethal dose and the dose that could be given daily without drastically affecting bone marrow.19
By chance, Dougherty had implanted a mouse with lymphoma, and the tumor was fairly advanced. Lymphoma tumors had little tendency to metastasize. They grew to an enormous size, often weighing as much as the mouse at the time of death.16,19 Lymphoma, therefore, was an ideal model for testing anticancer efficacy.
Not wanting to wait to establish a whole group of tumor-bearing mice, they gave nitrogen mustard to this single mouse. After just two daily doses, the tumor had softened and begun to shrink. It eventually disappeared. They stopped treatment, and the remission lasted about a month.19
When they detected a slight re-growth of the tumor, they treated the mouse again. The tumor shrank again, but not as completely as the first time. When it began regrowing, further treatments had no effect.19
The typical lifespan of a mouse following a lymphoma implant was about three weeks. The mustard-treated mouse lived for 84 days following implantation.19
Following this, Goodman and Gilman treated various tumors in mice, adjusting the dose, number of administrations, etc., attempting to optimize the dosing regimen. Many of these tumors regressed, but not all, and none completely disappeared like the original mouse’s tumor.19 These mouse experiments were never published, but the results were sufficiently encouraging to consider a therapeutic trial in people.16
The consortium of wartime researchers had compiled a comprehensive pharmacological profile of nitrogen mustard.16 They knew the bone marrow suppression was completely reversible, and there was a fairly wide safety margin between the effect on lymphoid tissue and the acute lethal dose.19
Also, they knew that thiosulfate was an effective, although imperfect, antidote.19 All of this raised Goodman and Gilman’s confidence that they could safely move forward with a clinical trial, despite nitrogen mustard’s classification as a poison.
The Pivotal Patient
Up to the 1940s, surgery and radiation were the only cancer treatment options.11,18 Most physicians thought that treating cancer with a drug (other than painkillers) was akin to malpractice.19
But when Gilman showed the data to Gustaf Lindskog, he was impressed. Lindskog, an assistant professor of surgery at Yale, thought any drug with promise of controlling cancer (even a cytotoxic compound like nitrogen mustard) was worth trying.13,19 He agreed to supervise the trial, and he soon identified a suitable patient.
JD was 47 when a couple of rapidly growing masses appeared beneath his jawbone. Those fluid-filled masses were removed, but they soon reappeared, and JD could barely open his mouth. A biopsy confirmed that the neck tumor was a lymphosarcoma, and JD entered Yale Medical Center for X-ray therapy on February 23, 1941.22
Radiation treatment initially shrank the tumor, but eventually the lymphosarcoma spread to his lymph nodes, creating large masses in his armpits. Repeated radiation helped, but by August 1942, JD had difficulty breathing and swallowing, and he had lost weight.22
Radiation was no longer effective, and surgery was out of the question. This type of cancer was known to be rapidly fatal, and the doctors considered JD’s condition “hopeless.”22
JD was not Gustaf Lindskog’s private patient, but he was interested in JD’s management and took responsibility for overseeing his care. On August 25, 1942, Lindskog presented JD’s case to the Yale Tumor Conference. The committee agreed that JD had no other therapeutic options and gave Lindskog permission to begin treatment with the experimental compound.22 Because Goodman and Gilman’s work was still classified, nitrogen mustard was referred to exclusively as “substance X.”8,22
Lindskog fully explained the situation to JD, who understood that all conventional treatments had been exhausted and that “substance X” was experimental. Lindskog said that JD “readily agreed to accept the chance for help, whatever the risk.”22
At 10:00 a.m. on August 27, 1942, JD received the first dose of “substance X.” It was an intravenous injection of 0.1 mg/kg.19,22 The dose had been extrapolated from the studies in rabbits and mice, and it was roughly 2.5 times what would become the standard dose.18 Unfortunately, the animal studies had not optimized the duration of therapy. They decided to give JD 10 daily injections.22
By August 31 (day 3 after the first dose), JD was feeling better and able to sleep, eat, move his head, and cross his arms across his chest. His condition continued to improve, but on September 6, his white blood cell count had fallen from 10,000 to 5,000 (barely within the normal range). Two days later, his white blood cell count dropped to 1,300. His platelet count was 22,000 (normal range is 200,000–500,000), and his gums began to bleed. He was given a unit of whole blood on September 21, and his blood counts recovered.22
On September 27 (day 31), all of JD’s neck and armpit tumors had disappeared. Unfortunately, JD experienced sporadic fevers and coughing, and his white blood cell count had dropped to 200–400. He was given another transfusion on September 30, and his white cell count rebounded to 2,200.22
In October and November 1942, JD received additional rounds of “substance X” infusions, which produced dramatic but short-lived regressions. Unfortunately, he also experienced profound bone marrow depression, bleeding gums and multiple peripheral hematomas. JD died on December 1, 1942 (day 96); however, the discoveries observed by Goodman and Gilman was considered a medical milestone.22
Goodman, Gilman and Lindskog had demonstrated, for the first time, successful chemotherapy treatment of a cancer patient.7 But in addition to inducing tumor regression, they also showed that resistance to chemotherapy could occur after multiple doses, and that chemotherapy could cause profound bone marrow suppression, immunosuppression, and death.22
The Yale Clinical Trial
In their enthusiasm (and what Gilman later admitted was “a serious error”), the Yale team began treating a second patient before JD had completed his first series of injections.19 By the time they fully appreciated JD’s profound bone marrow depression, they had completed the 10-day treatment of the second patient. This patient’s white blood cell count decreased, but unfortunately his tumor did not respond to treatment.16,19
The Yale group treated five additional patients using more conservative therapeutic regimens.16 All of these patients were in the terminal stages of various cancers, and the results were similar to what Goodman and Gilman had seen in mice with various tumors.19 Some patients responded, but none of them achieved the complete remission they had seen in JD.
Like the animal responses, the patients’ tumors reappeared as the bone marrow recovered, and there was no long-lasting cure.13,16 Considering that all of these patients had no therapeutic alternatives, the results were nevertheless encouraging and justified further clinical experimentation.
In June 1943, the Yale group dispersed.13,19 Gilman joined the U.S. Army and went to Edgewood Arsenal to work in the Chemical Warfare Service.2
Goodman went to the University of Vermont, where he headed the Department of Pharmacology and Physiology.3,6,23 In 1944, he moved to Salt Lake City to become the founding chairman of the Department of Pharmacology and was instrumental in building the full, four-year medical school curriculum at the University of Utah.5,6,23
Lindskog stayed at Yale, eventually became chairman of surgery, and was widely recognized for his contributions to thoracic surgery.3,18
Further Clinical Trials
After the Yale investigation, three other academic institutions with wartime government contracts conducted clinical trials with the nitrogen mustards.21
At the University of Utah, Louis Goodman coordinated the work of a team of clinicians, who recruited 34 patients at Salt Lake County General Hospital and 16 at Tufts Medical School. He also convinced his brother, Morton, a physician at the University of Oregon Medical School, to treat 10 patients.24
Lenn Jacobsen led the University of Chicago group, who treated 59 terminally ill cancer patients. David Karnofsky treated patients at Memorial Hospital in New York.8
Their greatest challenge was establishing a regimen that would kill cancer cells completely but preserve enough of the bone marrow to regenerate healthy blood cells. In addition, they tried to determine which types of cancer would be most susceptible to nitrogen mustard therapy.13
The Utah, Chicago and New York clinical groups treated a total of 160 patients, most of whom suffered from Hodgkin’s disease, lymphosarcoma or leukemia. After dose-ranging studies, they settled on a four-day course of treatment with 0.1 mg/kg. But despite their best efforts, the toxic effect of nitrogen mustard on white blood cell counts was “usually evident,” and loss of platelets caused bleeding gums. Other common side effects included nausea and vomiting, damage to blood-forming organs, and sometimes anorexia, weight loss, weakness and headaches.16,17,21
Patients with Hodgkin’s disease, which at that time was invariably fatal, responded most favorably to treatment.16,21 Many of them experienced rapid remissions, including some patients who no longer responded to radiation treatment. The remissions typically lasted 4–8 months.16,17,21,24 Enlarged lymph nodes, spleen, and liver decreased. In addition, most patients enjoyed a better quality of life (increased appetite, weight, strength, and sense of well-being).16,21,24
Less favorable results were obtained in treating lymphosarcoma, which is characterized by elevated lymphocytes and enlarged lymph nodes. Some patients, like JD, responded similarly to those with Hodgkin’s disease. But in many cases, nitrogen mustard treatment failed, and the investigators could not determine why some patients benefitted and others did not.16,21,24
A few patients with chronic leukemia showed modest improvement, but the results with acute leukemia were “disappointing.”16,24
These findings did little more than confirm the clinical results at Yale. The greatest effect of the nitrogen mustards was always on rapidly proliferating tissues, whether normal or cancerous. Unfortunately, nitrogen mustard was no cure. All patients eventually relapsed.16,17,21,24
The Italian Connection
Despite the extensive research and protective countermeasures, chemical weapons were not used by either side during World War II.11,13 But there was one massive accidental exposure.
As the Allied forces drove north in Italy, they established a storage depot at the port of Bari on the Adriatic coast.11,25 Mustard gas was stored in special ammunition dumps, ready to retaliate in case of a chemical attack.8
In the fall of 1943, Bari Harbor was crowded with supply ships and merchant vessels. Included in this flotilla was the USS John Harvey, a Liberty ship laden with ammunition, gasoline, military supplies, and a secret cargo of 2,000 chemical bombs.11,14,25 Each bomb contained 60–70 pounds of sulfur mustard.13
On December 2, 1943, Bari Harbor was attacked by German bombers. Although the air raid lasted only 20 minutes, 17 Allied ships were sunk. The John Harvey took a direct hit, setting off a chain reaction of ammunition explosions in its cargo bay and releasing sulfur mustard from some of the broken mustard bombs. Everyone aboard the John Harvey perished, including the specialists who knew about the secret cargo and had been trained to safely handle chemical weapons.8,11,13,25
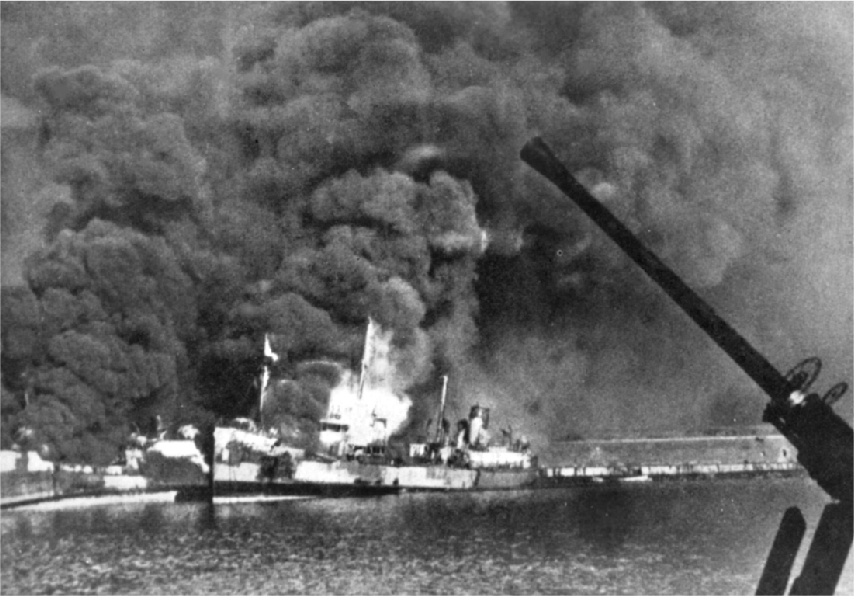
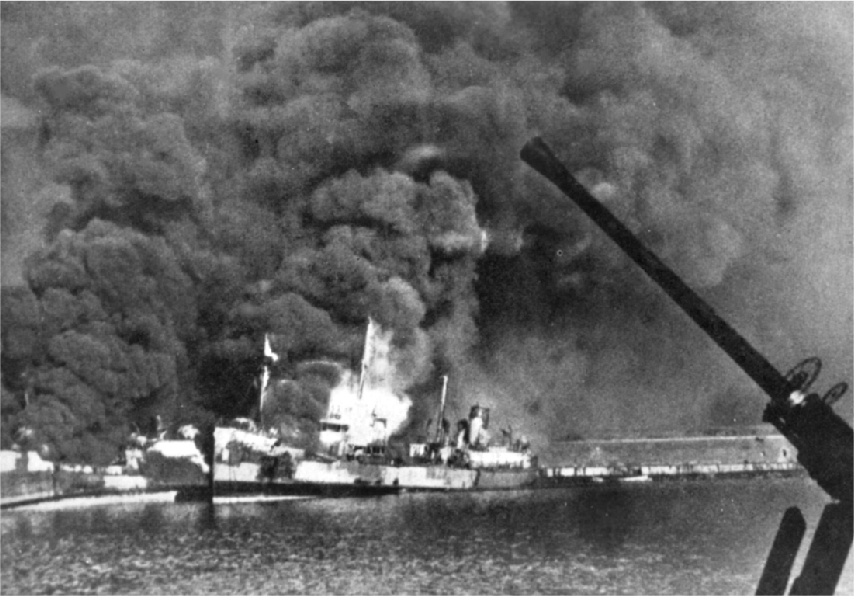
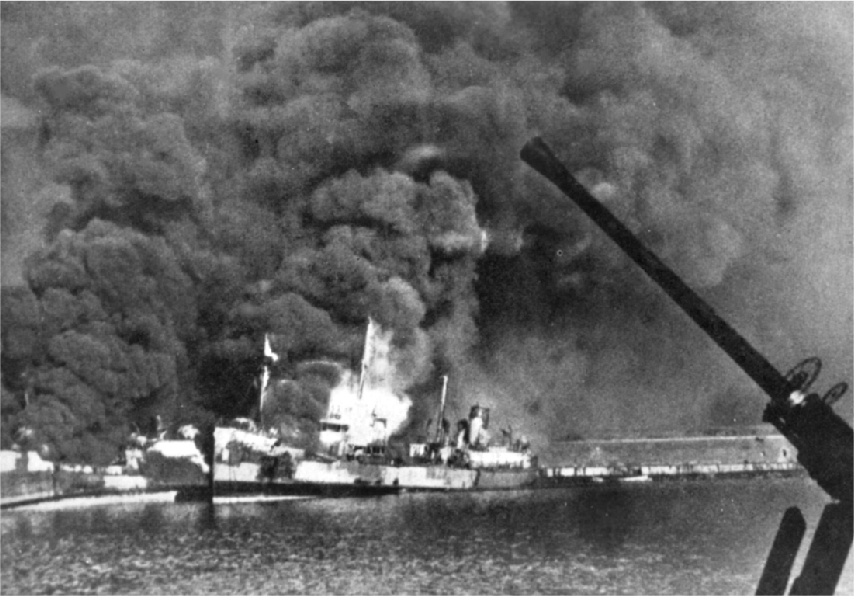
Some of the sulfur mustard vaporized, exposing personnel aboard the burning ships, in rescue vessels, and at the field hospitals. By the next morning, these casualties began showing the signs and symptoms of mustard gas poisoning, which were well-known from World War I: eye irritation, skin blistering, and lung inflammation.25
Gasoline and fuel oil gushed from the ships and flooded the harbor, creating a thick oily slick.13,25 Liquid sulfur mustard that was not burned mixed and dissolved in the oil slick. Many sailors and merchantmen jumped or were thrown from their damaged ships. The soaking wet men who showed no obvious signs of blast injuries sat unattended for hours in the field hospitals.25
Unfortunately, extended exposure of the skin to sulfur mustard in their wet clothes provided ideal conditions for systemic absorption of the chemical.25 Over the next few days, these men exhibited a syndrome unlike the World War I victims but strikingly similar to the effects already documented by Goodman and Gilman at Yale and Alexander’s group at Edgewood Arsenal.
The victims’ white blood cell counts dropped as low as 100. Not all of the mustard-exposed casualties suffered a fall in white blood cell counts, but all of those with extremely low counts died. At autopsy, these victims had small, shrunken spleens, pale lymph nodes and bone marrow devoid of its normal red color.25
At this time, Stewart Alexander had been posted to the Allied Headquarters in Algiers as General Eisenhower’s personal consultant on chemical warfare and the care and treatment of chemical casualties. As the casualties mounted in Bari, Alexander was dispatched as a medical advisor.8
By the time he arrived in Bari on December 7, 1943, many of the patients were suffering mustard poisoning too severe for any treatment to reverse.8,25 He could only offer medical advice to optimize nursing care. He carefully reviewed all of the patients’ medical records, ordered additional laboratory tests, preserved tissue samples and ensured that this accidental chemical exposure was thoroughly documented.8
Of the 617 Bari casualties exposed to sulfur mustard, 83 died. This death rate (~14%) was much higher than the 2% fatalities from mustard gas in World War I. The major difference was the severe physiological damage caused by systemic absorption of the oily mustard solution.25
Although unfortunate, this large-scale accidental exposure provided an independent confirmation of the cytotoxic effects that Goodman, Gilman, and the other investigators had seen in their clinical trials of nitrogen mustard.
Published at Last
During the war, chemical weapons researchers filed their results in classified documents, which were circulated to only a limited number of people with the proper security clearance. Beginning in 1946, they were permitted to publish their work in the open literature.11,16,21,24,25
Goodman and Gilman published the results of their seven Yale patients in JAMA on September 21, 1946.24 This report documented the 1942 treatment of JD, the first cancer patient successfully treated with a chemical. Goodman and Gilman were universally hailed as the pioneers of cancer chemotherapy.1,6,8,11,12,14,18,22
Lenn Jacobson at the University of Chicago, David Karnofsky at New York’s Memorial Hospital, and Stewart Alexander also published their findings.17,21,25 All of these wartime investigators acknowledged that their results were preliminary. They urged further clinical trials to confirm which types of cancer would respond best to nitrogen mustard treatment.
The National Research Council offered free nitrogen mustard “to qualified institutions for investigational purposes.”21 Many researchers requested it.11 In 1949 the Food and Drug Administration approved the use of nitrogen mustard to treat cancer, despite its side effects and short duration of action.7
Wartime clinical studies had been conducted using two nitrogen mustards: bis(2-chloroethyl) methylamine and tris(2-chloroethyl) amine. Both were the product of a screening program designed to find the most potent chemical warfare weapons, not therapeutic drugs.16,21
After the war, chemists synthesized hundreds of analogs, hoping to find compounds that had a wider safety margin and a longer duration of action.7,12,19,21,24 They found that adding an aromatic side chain to the nitrogen mustard backbone produced compounds that were more stable and had more favorable pharmacological properties.12
The first clinically useful analog was chlorambucil, which was introduced in 1953.12,20 Cyclophosphamide (the most successful and widely used nitrogen mustard) was introduced in 1958. These analogs could be taken orally, a significant advantage. They were well tolerated in small daily doses and provided flexible titration, which avoided depletion of blood cell counts.21,26
The aromatic nitrogen mustard analogs soon formed the cornerstone of anticancer treatment and are now routinely incorporated into multidrug chemotherapy.12,13,18
Louis Goodman remained at the University of Utah for the rest of his career. In 1949, he became the founding editor of ASPET’s newly launched “Pharmacological Reviews.”
The Second Edition
Louis Goodman remained at the University of Utah for the rest of his career. In 1949, he became the founding editor of ASPET’s newly launched Pharmacological Reviews.2,6,7
After Alfred Gilman’s discharge from the Army, he joined the College of Physicians and Surgeons at Columbia University as a professor of pharmacology. In 1956, he became the founding chairman of the Pharmacology Department at the newly established Albert Einstein College of Medicine. In 1973, Gilman returned to Yale as a lecturer in pharmacology.2,3,23
Goodman and Gilman realized that an updated edition of their textbook was long overdue. The first edition had contained three chapters describing the treatment of syphilis with arsenic, bismuth, and mercury. There were only cursory references to cancer treatment with painkillers.6
The intensive investment in wartime research produced advances in pharmacology that also benefited peacetime patients, such as chloroquine for malaria and mass production of penicillin, as well as nitrogen mustards for cancer.2,13 This explosion in pharmacology subject matter continued after the war and made updating the textbook challenging. By the time they finished a section of the book,
it was already out of date. They rewrote some chapters multiple times.2,4
In 1955, after nearly a decade of repeated revisions, the second edition of the textbook was finally published. It included descriptions of newly introduced drugs: nitrogen mustard and other anticancer drugs, the first effective treatments for hypertension, the first antihistamines, the first antibiotics (penicillin, streptomycin, tetracycline, and chloramphenicol), and new diuretics.6 In addition, Goodman and Gilman incorporated the cellular mechanisms of action for the older drugs.4
They realized that they could not keep up with the rapidly expanding pharmacology literature for future editions of the book, alongside the demands of their regular jobs. For the third edition, they invited 42 trusted colleagues and former students to write the various chapters.2,4 But Goodman and Gilman maintained tight control over the quality of the text and were actively involved as the book’s editors.
Now in its 14th edition, the textbook’s section on alkylating agents begins with: “In 1942, Louis Goodman and Alfred Gilman, the originators of this text, demonstrated the activity of nitrogen mustards against mouse lymphoma. Their clinical studies of intravenous nitrogen mustards in patients with lymphoma launched the modern era of cancer chemotherapy.”26
The two coauthors maintained a long-distance friendship, connected by their textbook’s many editions. But they pursued separate research interests. They frequently served as consultants and advisors, and among their many honors was election to the National Academy of Sciences. Goodman served as president of ASPET in 1959, and Gilman followed as president in 1960.2
In a 1980 interview Goodman reminisced, “We bonded like brothers, never quarreled, had a lot of fun, and learned from each other.”5
Goodman served as ASPET president in 1959, and Gilman followed as president in 1960.
Author
-


Rebecca J. Anderson holds a bachelor’s in chemistry from Coe College and earned her doctorate in pharmacology from Georgetown University. She has 25 years of experience in pharmaceutical research and development and now works as a technical writer. Her most recent book is Nevirapine and the Quest to End Pediatric AIDS.
View all posts