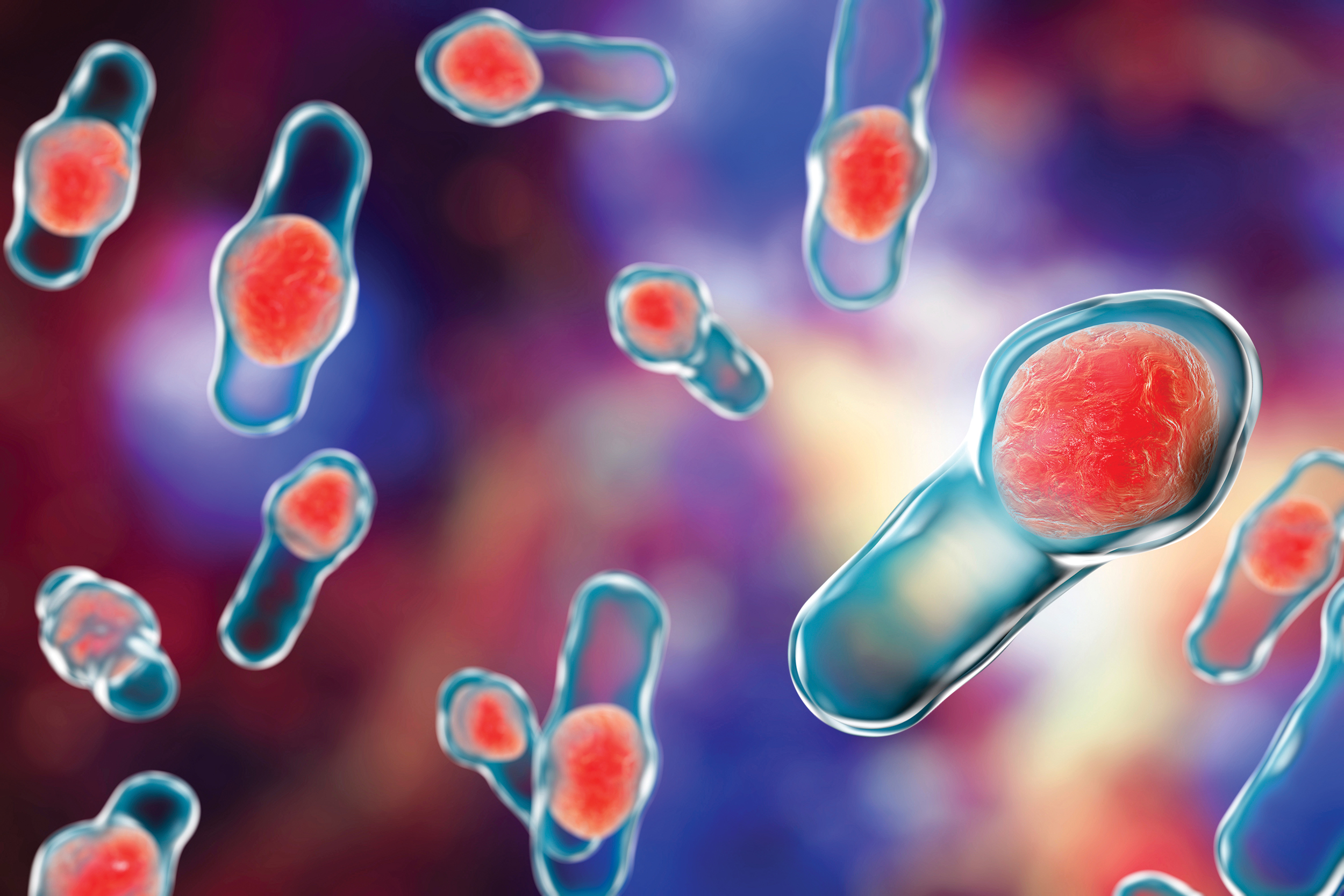
3D illustration of Recurrent Clostridium difficile bacteria
When we go to the doctor with an earache, urinary tract infection, or bacterial pneumonia, we expect to get an antibiotic. Doctors could take a swab and do a culture to identify the specific microbe and then prescribe a targeted drug to kill it. But that takes several days, during which we continue to suffer, and the infection might progress to serious complications. Instead, doctors usually prescribe a broad-spectrum antibiotic, and the odds are good that we will immediately feel much better.
The downside, of course, is that this shotgun approach contributes to the development of resistant bacterial strains. A broad-spectrum antibiotic also takes out a lot of innocent bacteria, including some of the “good guys” in our gastrointestinal tract. To compensate for that (and the accompanying antibiotic-induced diarrhea), the doctor may also instruct us to eat a reasonable amount of yogurt, a probiotic that helps repopulate our gut microbes.
This strategy usually works. But in some cases, particularly in hospitalized, immunocompromised, and elderly people, or when patients take broad-spectrum antibiotics long-term, the diarrhea gets out of control, beyond the ability of even the most potent probiotic yogurt. This condition is called pseudomembranous colitis, and in most cases, the culprit is a toxin produced by Clostridium difficile.
Pseudo Membranes
In 1893, J.M.T. Finney was the first to report pseudomembranous colitis. He observed changes in the intestinal lining of a 22-year-old postoperative patient who was being treated by the renowned Johns Hopkins physician, William Osler.1–3
Pseudomembranous colitis is an anatomically identified inflammation of the colon. Yellow-white plaques emerge to form an elevated “pseudomembrane” on the mucosal lining of the intestine.
Pseudomembranous colitis can result from a variety of conditions including Crohn’s disease, ulcerative colitis, irritable bowel syndrome, intestinal obstruction, colon cancer, leukemia, severe burns, shock, uremia, heavy metal poisoning, hemolytic-uremic syndrome, shigellosis, neonatal necrotizing enterocolitis, ischemic colitis, and Hirschsprung disease.1,4
In the early 1950s, pseudomembranous colitis (and the accompanying diarrhea) became recognized as a common complication of antibiotic use.1,2
The Clostridium Connection
Clostridium difficile was first isolated from the stool of a healthy infant by Hall and O’Toole in 1935.1,3,5 The name reflected the difficulty they had in culturing and isolating it.3 They found that C. difficile produced a toxin that was highly lethal to mice. It was between 10- and 100-fold less toxic than the extremely potent toxin produced by botulinum bacteria.1
C. difficile is a Gram-positive bacterium and a normal constituent in the gut.6,7 It is one of more than 200 genera in the Firmicutes phylum, which along with Bacteroidetes, comprises 90% of the gut microbiota.8,9
Gut microbes promote digestion by producing metabolites including short-chain fatty acids, assist absorption of nutrients, support the synthesis of essential vitamins like vitamin B, promote enzymatic activity of the mucosa, provide a barrier to pathogens and toxins, play a protective role in assisting the immune system, and even metabolize some drugs.4,7,8 In a healthy gut, the spore-forming bacteria of the Firmicutes phylum play an important role in controlling the growth of C. difficile.2,7,9
In 1978, W Lance George and colleagues at UCLA discovered the connection between C. difficile and pseudomembranous colitis. When a broad-spectrum antibiotic disrupts the delicate balance of gut flora, pathogenic strains of C. difficile have the opportunity to colonize, dominate, and produce two toxins, A and B.2,5,7,10
Those toxins inflame the colonic epithelium, leading to clinical symptoms varying from mild diarrhea to severe life-threatening pseudomembranous colitis.1,5 Although it can result from many other conditions, the leading cause of pseudomembranous colitis and antibiotic-induced diarrhea is now C. difficile. It accounts for more than 450,000 cases in the U.S. each year.1–3,5–7,11 And as antibiotic use has increased, so has the incidence of C. difficile colitis.
The fundamental problem is not the presence of C. difficile per se, but rather the absence of healthy flora to keep its growth in check. Mild cases of C. difficile infection require little more than supportive measures and discontinuation of antimicrobials. Those patients experience no further symptoms.2,5,12
But if unchecked, C. difficile can take over the large intestine. In severe cases (characterized by pseudomembranous colitis), patients experience watery diarrhea and as many as 15–30 bowel movements per day. Diarrhea and colitis can last for weeks or months.1,2,6
C. difficile infection has become the leading cause of hospital-acquired disease.3,5,12 Other risk factors are age (over 65 years) and immunosuppression.1,13 C. difficile colitis mortality rates as high as 24% have been reported in critically ill patients. It accounts for more than 20,000 deaths in the U.S. each year.2,3,6,11,12
Although it can result from many other conditions, the leading cause of pseudomembranous colitis and antibiotic-induced diarrhea is now C. difficile.
First Line Treatment
Early work using a cell cytotoxicity assay to detect C. difficile toxin B confirmed that antibiotics (specifically vancomycin and metronidazole) would inhibit pseudomembranous colitis in a hamster model of C. difficile infection. This provided the rationale for treating C. difficile infected patients.1
Currently, an initial episode of C. difficile infection is treated with oral fidaxomicin (preferred), vancomycin, or metronidazole.13,14 Fidaxomicin has a narrow spectrum of activity, which limits its effect on the gut microbiome and is associated with higher rates of sustained response and fewer recurrences.13,15,16
Unfortunately, C. difficile infection is sometimes difficult to control. Up to 35% of patients experience recurrence of diarrhea after this course of antibiotic treatment.2,4,5,10,12–14,17
Recurrent C. difficile infection is treated with bezlotoxumab (an anti-C. difficile toxin B antibody), along with a more aggressive pulsed or tapered regimen of antibiotics.2,4,5,12,17 Adding bezlotoxumab to antibiotic therapy is especially recommended in patients who have risk factors for recurrence (e.g., ≥ 65 years old, severe C. difficile infection, or immunosuppression).13
For many patients, this course of treatment is successful. But repeated use of antibiotics may predispose patients to further relapses and chronic, recurrent C. difficile colitis.2,10 After three recurrent episodes, patients have up to a 65% chance of additional recurrences, despite antibiotic treatment.5,10,12,16,17
Possible explanations for the recurrences are: persistence of C. difficile spores, diminished response to the toxin B antibody, and persistent intestinal disturbance caused by the reduced diversity of the gut flora.5,14
There are 200,000 cases of recurrent C. difficile infection in the U.S. each year.18 And the risk of multiple recurrences has increased in recent years.5,13 Some of those multiple relapse cases are incredibly debilitating and extremely difficult to stop without continuous antibiotic therapy.1
Alternatives to antibiotics have been explored, including immunoglobulins, probiotics, bile salt binding resins (cholestyramine), toxin-binding molecules, C. difficile vaccines, and whey prepared from vaccinated cows.1,4,5,10,12 Unfortunately, none of these has proven to be effective.1,4
Repeated use of antibiotics may predispose patients to further relapses and chronic, recurrent C. difficile colitis.
A Rationale for Recycling
In 1958 (before C. difficile was recognized as the diarrhea-producing culprit), Ben Eiseman, the Chief of Surgery at Denver General Hospital, and his colleagues used enemas of donor feces to successfully treat four patients who had pseudomembranous colitis.5,7,19
A few historical references describe the benefits of this type of treatment. The oldest account dates to the 4th century, when a Chinese physician, Ge Hong, advised consuming fresh stool from a healthy neighbor for those suffering from food poisoning or severe diarrhea.19 The fecal suspension was called “yellow soup”.7 But Eiseman’s rationale probably came from the extensively documented reports of animals that benefit from consuming fecal matter.10
In the 17th century, the Italian anatomist, Fabricius Aquapendente, reported feeding viable enteric bacteria to animals that had lost their ability to ruminate. A portion of cud that had already been chewed by a healthy ruminant animal was fed to the sick animal, which immediately stimulated chewing and restored its health.10
Dogs eat poop because they are craving something in the feces that is missing in their existing diet. A similar behavior is seen among rodents and birds.20
Some species, for example baby rabbits and panda cubs, rely heavily on their parents’ poop. The parents’ poop inoculates the offspring’s immature gut microbiome and may be the only way their intestinal tract can obtain highly specialized, species-specific microorganisms.20,21
Cross-species fecal ingestion might also work. In World War II, German soldiers in the Afrika Corps consumed fresh, warm camel feces, which was recommended by local Bedouins as a remedy for bacterial dysentery.7,21 Efficacy was probably due to the antibiotic subtilisin, generated by Bacillus subtilis in the camel’s feces.21
FMT
Following Eiseman’s initial report, and especially after recognition that antibiotic-induced diarrhea was caused by C. difficile, there was a sound rationale for using a procedure that reintroduced “healthy” gut microbes to ailing patients.
Dozens of researchers confirmed Eiseman’s success by administering human fecal matter to patients with C. difficile infections in a procedure that is generally referred to as fecal microbiota transplantation (FMT). Most of the published reports were case studies involving only a few patients each.
Because these were all exploratory studies, the FMT protocols, not surprisingly, varied regarding the type of donor, preparation of
the stool, pretreatment(s) of the recipients, routes of administration, endpoints, and duration of follow up.
Initially, investigators recruited donors who were closely related to the recipient. The order of preference was domestic partners, family members, those living in the same household, and finally close friends.4,5,12,22 The theoretical rationale was that intimate contact between the donor and recipient raised the likelihood that pathogens and flora would have already been shared between them and minimized the risk of transmitting new pathogens.2,10,12,23
But there was no rationale for excluding unrelated healthy volunteers.5 Some investigators successfully recruited medical students, surgical residents, and unrelated healthy individuals as donors.10
Regardless of the source, most investigators took great care to ensure that the donated stool was free of pathogens. Many of them employed the procedures that are used to screen transplant donors and their donated organs.10 The donors’ blood was tested for antibodies to HIV, hepatitis, cytomegalovirus, Epstein-Barr virus, etc. Their stool was screened for common transmissible diseases including parasites, C. difficile, and enteropathogenic bacteria.12,14,23 The procedures might also include culturing successive stool specimens and/or microscopically confirming that the stool was negative for protozoa, worms, and ova.10
The microbial viability of fresh fecal samples is about 6 hours, which meant that the laborious screening of donors and the donated stool was logistically challenging.15 Typically, investigators timed the donation so that the FMT was prepared and administered on the same day that the stool was collected.4,5,10,12,14
The donated stool was usually homogenized with water or normal saline and filtered to remove particulate matter.4,5,12 The resulting slurry needed to be sufficiently liquid to pass through a tube, but the amount of water was minimized to ensure maximal microbial concentration. The volume was generally 200 to 300 ml and contained up to 300 grams of donor stool.4,10,12
The slurry was administered upward by an enema or through a colonoscope, or downward through a gastroscope, nasogastric tube, or nasojejunal tube.
The microbial viability of fresh fecal samples is about 6 hours, which meant that the laborious screening of donors and the donated stool was logistically challenging.
Frozen Capsules
The logistical challenges of preparing fresh stool suspensions from related donors hindered the development of a widely applicable treatment protocol.15 In addition, administration by intubation or colonoscope required the appropriate clinical facilities and medical expertise.
To circumvent these difficulties, a group at Massachusetts General Hospital developed a frozen capsule form of FMT that could be prepared in advance, stored for reasonable periods, and administered orally.15
After the donors and their donated stool were screened for pathogens, the filtered slurry was concentrated by centrifugation and pipetted into capsules, which were then secondarily sealed inside slightly larger capsules. The capsules were stored in an ultracold freezer. The total dose (15 thawed capsules on each of 2 consecutive days) contained about 48 grams of concentrated fecal material derived from a single donor.15
This procedure allowed healthy volunteer donors to be screened in advance, and storage of the frozen material permitted retesting of donors, if necessary, which further increased the safety of the procedure.
There was also the convenience factor. Colonoscopy and intubation delivery are invasive, resource intensive, costly, and need to be administered by specialists in a clinic or hospital. By contrast, oral capsules could be administered in an office setting.16
Oral capsules provided the same benefits as the infusion methods with less of an “ick” factor.6 Despite the “lack of aesthetic appeal,” the recipients rated their experience as “not at all unpleasant.”2,16
Uncontrolled Success
FMT efficacy was typically defined as resolution of diarrhea without relapse, and the outcomes were dramatic.2,14 In most cases, the patients felt much better (that is, marked resolution of symptoms) within 12–24 hours. Their bowel habits soon returned to what they had been prior to their first episode of C. difficile colitis.2,5,23
More than 75% of treated patients were symptom-free after a single FMT infusion.7,16 Sometimes, a second or third FMT infusion was required, and the overall efficacy rate (after one or more treatments) rose to above 90% of treated patients.2,5,16,19,22 Impressive efficacy was also achieved in immunocompromised, severely ill, and elderly patients. By contrast, standard antibiotic regimens benefited only 30% of them.19
Analysis showed that the FMT recipients’ fecal bacterial diversity had increased, similar to that of healthy donors.4,14 Patients who had been diagnosed with pseudomembranous colitis not only experienced resolution of their diarrhea but also the pseudomembrane in their colon disappeared.10
The precise mechanisms of action of FMT are unclear but probably involve recolonization of flora with missing components, which restores the gut microbial balance and reestablishes the host-defense against C. difficile colonization.4,5,7,10,12
Another major mechanism could be the direct antagonistic activity of the normal flora to C. difficile. Bacteria-generated bacteriocins, for example, possess powerful antimicrobial properties. This view is supported by in vitro studies, which showed that normal fecal flora antagonize C. difficile.10 These microbiome-generated substances seem to have the added power of eliminating bacterial spores, which antibiotics cannot eradicate.23 So, organisms in the FMT not only cure the current infection, but also prevent future germination and colonization of the hardy C. difficile spores.10
Most investigators reported that FMT-treated patients remained symptom-free for the duration of follow up, which varied from 5, 10, 13, to 16 years, depending on the case study.10,12,19,23 Patients who remained symptom-free at the end of the study’s follow up period were considered “cured.” Those FMT-treated patients who redeveloped C. difficile infections typically had been prescribed antibiotics for unrelated infections and were considered reinfections rather than relapses.12
Not only was the efficacy of FMT impressive, but also the procedure was remarkably safe.4 The only side effects reported by recipients were mild to moderate cramping, belching, bloating, flatulence, or abdominal distension on the day of treatment.5,14,15,17 In most patients, these effects were self-limiting and resolved within a few hours or a few days.14,15,17 Transmission of communicable diseases was not observed in any patient.19
Controlling Treatment
Several authors reviewed and summarized the reports published by researchers more than 30 years and which covered the results of more than a thousand patients.4,5,7,10,19,24 Their meta-analysis of these exploratory studies showed that efficacy was “dose” dependent, with FMT volumes of 500 ml consistently providing around 90% cure rates.4,14,16
When an optimal FMT dose was administered, the analysis showed that there was no difference in efficacy regardless of the route of administration: enema, colonoscope, nasogastric tube, nasojejunal tube, or oral capsules.7,12,15,16,23,24 Efficacy was also the same, whether the donor was a domestic partner or unrelated to the recipient, and frozen preparations were equally effective as freshly prepared stool samples.16,24
Although these accumulated case studies built impressive circumstantial evidence supporting the efficacy and safety of FMT, randomized, placebo-controlled trials were lacking. For one thing, it was difficult to find a suitable placebo resembling fecal matter.10 On the other hand, some investigators rationalized that the uncontrolled results were so impressive, and recurrent C. difficile infections were otherwise so difficult to treat, that a “placebo effect” was unlikely.12
The first randomized controlled trial of FMT was published in 2013 by a Dutch group led by Els van Nood.14 This open-label study was stopped after the interim analysis, because most patients in the control groups (receiving vancomycin and bowel lavage) had relapsed.14
The results showed that FMT was significantly more effective for treating recurrent C. difficile infection than vancomycin treatment. The overall cure rate in the FMT group was 94%. Also, the investigators saw increased fecal bacterial diversity in the FMT recipients, similar to that in healthy donors.14
Analysis of 7 subsequent randomized controlled trials reported equally impressive cure rates.24
When an optimal FMT dose was administered, the analysis showed that there was no difference in efficacy regardless of the route of administration: enema, colonoscope, nasogastric tube, nasojejunal tube, or oral capsules.
Stool Banks
As the demand for FMT grew, not all interested physicians had the facilities to screen and prepare stool donations. To meet the growing need, stool banks were established.25
In 2013, OpenBiome was founded as an independent nonprofit stool bank (run out of a laboratory at the Massachusetts Institute of Technology) to provide FMT samples for investigational purposes. Healthy volunteers were examined by internal medicine physician and underwent a series of laboratory tests. The stools of qualified donors were kept in quarantine until all assessments (clinical, serological testing, etc.) had been completed.7 Qualified stools were then prepared, and the slurry was stored in a freezer until it was shipped to the investigator for infusion by colonoscopy or enema.
Over the following decade, OpenBiome supplied more than 60,000 FMT preparations to clinicians and investigators.6
In 2013, OpenBiome was founded as an independent nonprofit stool bank to provide FMT samples for investigational purposes.
DIY—Homemade FMT
FMT was so simple that some desperate patients took the initiative to prepare homemade FMT by collecting stools from family or friends and making the slurry with their kitchen blender and coffee filter paper.25 Do-it-yourself videos of the procedure were posted on YouTube.
Individual investigators and stool banks like OpenBiome took great care in screening donors, but the screening procedures were not standardized or regulated.25 Furthermore, unlike these scientists, the do-it-yourselfers probably lacked an appreciation of possible disease transmission and also lacked the proper facilities to screen for pathogens.6
The Food and Drug Administration (FDA) and ethically minded investigators grew increasingly concerned that the wide-ranging quality controls and lack of regulatory standards posed serious safety risks. Without those guardrails, there was the potential for exposing unsuspecting patients to potentially dangerous fecal pathogens.6
Despite a recognized need for policy and guidelines, the FDA was uncertain how to regulate FMT. Was it a drug or a bodily tissue? Like a drug, FMT consisted of microbes in feces that changed how the body functions. On the other hand, because of those very microbes, FMT was like a biological tissue.6
FMT is also a method and could be evaluated as a procedure. FDA regulates procedures (for example, tissue and organ transplants) according to an entirely different set of rules. Then again, FMT could be considered a combination drug and delivery system, similar to an EpiPen or asthma inhaler.6
Regulating FMT
The FDA was reluctant to create a new regulatory product category, just to address FMT. Instead, regulators mulled over how to fit it into one of the existing regulated product categories.6
In 2013, FDA had to make some firm decisions, because a couple of companies filed Investigational New Drug (IND) Applications. Those companies, Ferring Pharmaceuticals and Seres Therapeutics, wanted to begin formal clinical trials and intended to develop commercial FMT products.
The FDA officially categorized FMT as a biological for regulatory purposes.6 From that point on, FMT was considered “investigational,” and any physician wishing to perform the procedure needed to file an IND. Because INDs involve considerable paperwork, most practicing physicians were unable or unwilling to comply with this administrative burden. Many doctors with C. difficile infected patients spoke out against the new IND requirements.6
The FDA issued a guidance, which went back and forth in drafts and revisions for almost a decade. The final guidance was issued in 2022.26 FDA regulators indicated that they would regulate FMTs with a light touch and practice “enforcement discretion.” That is, they would politely look the other way regarding doctors who treated C. difficile infected patients with FMT outside the IND-clinical trial setting, as long as they followed specific guidelines (e.g., patient informed consent, donor and donated stool screening, FMT storage conditions, etc.).26
Stool banks, on the other hand, were required to comply with FDA’s Good Manufacturing Practices, and investigators using FMT from a stool bank needed to comply with IND requirements.26
During its monitoring, FDA received several reports of invasive infections in immunocompromised patients who had received an FMT product supplied by a stool bank.7 Consequently, in 2020, FDA and OpenBiome agreed to implement even stricter testing for pathogens such as E. coli toxins.7,26
Although no approved FMT product was yet commercially available, the American College of Gastroenterology issued guidelines in 2021 strongly recommending FMT for patients experiencing recurrent C. difficile infections.27 ACG admitted that the quality of the published clinical evidence was “moderate” or “low” (due few and small controlled trials) but acknowledged that clinical experience had repeatedly shown that the procedure yielded high cure rates.27
The ACG also set up a registry and encouraged physicians to enter data regarding short-term adverse outcomes and long-term safety concerns. This FMT National Registry is funded by the National Institutes of Health and aims to track 4000 FMT recipients for 10 years.
Also in 2021, OpenBiome began winding down its operations, because it appeared that FMT commercial products were nearing regulatory approval. Instead of continuing to produce its own FMT products, the company established a partnership with the University of Minnesota’s Microbiome Therapeutics Program. The University of Minnesota manufactured FMT preparations for OpenBiome under Good Manufacturing Practices. This supplemented OpenBiome’s ongoing stool bank service, which continued to supply FMT for investigational studies and filled the gap until the first commercial product was approved.18
Approved at Last
On November 9, 2022, the FDA approved Rebyota®, the first FMT product for treating recurrent C. difficile infections. Multiple outside experts testified that it would be beneficial to have a regulated product on the market.18 Not only had physicians given FMT treatments successfully for decades (which supported its efficacy and safety), but also do-it-yourselfers were proliferating, and physicians were increasingly concerned about the hazards of this unregulated activity.
Rebyota is a live fecal microbiota suspension of rigorously screened stools collected from healthy human volunteers.17,28 Each bag of fecal suspension contains the stool from a single donor and is stored in an ultracold freezer until shipped to the distributor or end user. It is thawed for 24 hours before administration.17,28,29 Treatment consists of a single 150 ml dose administered as an enema.29
In masked, placebo-controlled trials, 289 adults with recurrent C. difficile infection were randomized to receive Rebyota or placebo (normal saline), following a course of antibiotic treatment.28 The rate of treatment success (absence of diarrhea for 8 weeks) was 70.6% with Rebyota vs. 57.5% with the antibiotic-only placebo. More than 90% of patients who were symptom-free at 8 weeks remained symptom-free through 6 months.28
An Oral Option
On April 26, 2023, the FDA approved Vowst® for treating recurrent C. difficile infection in adults.11 Vowst is an oral capsule containing live fecal microbiota spores. It was the first orally administered microbiota-based suspension to be approved.13
Antibiotic-induced loss of beneficial Firmicutes bacteria enables C. difficile spores (which are not killed by antibiotics) to germinate, proliferate, and produce toxins, creating a cycle of recurrent disease.9
The rationale for Vowst is that purified spore-forming Firmicutes bacteria will inhibit C. difficile spore germination, compete metabolically with C. difficile for essential nutrients, modulate bile-acid profiles, and/or reestablish resistance to C. difficile colonization.9
The source material for Vowst is stool from healthy human donors.30 The stools are tested for a panel of transmissible pathogens and then treated with ethanol to kill fecal Firmicutes organisms but not their spores. The resulting spore-laden material is formulated to the desired spore concentration and filled in capsules that are then over-encapsulated.30 The product has a three-year shelf life when refrigerated. The recommended dose is four capsules daily for three consecutive days.13,30
The Phase 3 trial was double-blind, randomized, and placebo-controlled in 182 patients with recurrent C. difficile infection.9 The rate of treatment success (less than 3 bowel movements per day and symptom resolution) at 24 weeks was 78.7% in the Vowst group and 52.7% in the placebo group, which received only antibiotics.9,31 The investigators noted that one-third of patients in the placebo group dropped out before week eight, mostly due to recurrence of C. difficile infection.9
More Uses
FMT has been mostly applied to treat chronic recurrent C. difficile-associated diarrhea and pseudomembranous colitis. Scattered case reports have indicated that FMT also induces high remission rates or improvement of symptoms in patients with irritable bowel syndrome, ulcerative colitis, and inflammatory bowel disease.4,10,12,19,23
Inflammatory bowel disease and irritable bowel syndrome have been causally associated with disturbances in the composition of gut flora, but the specific bacterial pathogens in these conditions have not yet been identified.10,23 Consequently, probiotics or FMT (the ultimate therapeutic bacterial mixture) may have value in treating such disorders, especially when patients are refractory to other treatments.10
Because the results for these indications have been variable and the numbers of patients are low, the data are too limited to draw firm conclusions and establish treatment guidelines.19 It has been recommended that patients with inflammatory bowel disease or irritable bowel syndrome should be treated with FMT only within protocol-specific clinical trials.7,19
Since the 1990s, FMT has also been explored to treat many other conditions including chronic constipation, Crohn’s disease, metabolic syndrome, chronic fatigue syndrome, and even multiple sclerosis.19
In recent years, researchers have discovered that there are strong correlations between the gut microbiome and other parts of the body.7 Existing evidence suggests that disruption of gut microbes can contribute to numerous diseases including diabetes, atherosclerosis, atopic dermatitis, and autism.7 This provides some justification for FMT as a treatment option. Even without knowing the specific microbial species involved, healthy fecal bacteria may still counteract pathogen(s) and reestablish gut homeostasis.23
There are also anecdotal reports of people losing weight, or changing their dietary desires, after receiving FMT from a healthy donor.6 But at least one randomized clinical trial involving an FMT donor and obese recipients showed no weight loss effect.32
Because the gut’s metabolic activity and the brain are in constant bidirectional communication, a few clinical trials are researching FMT as a possible treatment for brain disorders such as depression, anxiety, Parkinson’s disease, Alzheimer’s disease, and sleep disorders.8
More than 200 FMT clinical studies for dozens of disease indications are registered in clinicaltrials.gov, a number of which are randomized controlled trials.
As one investigator said, “There are few medical therapies that reverse severe illness so dramatically.”
The Last Best Hope
Most patients with C. difficile infections can be effectively treated using targeted antibiotic regimens, which should remain the first line of therapy. For the subpopulation of patients with recurrent C. difficile-induced diarrhea despite repeated antibiotic therapy, FMT is a rational, and now approved, treatment.12
FMT has advantages over repeated antibiotic regimens, which may perpetuate or renew the disruption of gut flora. Also, FMT reduces the risk of antibiotic resistance and allergic reactions.2 It may not be perfect, but the procedure is easy, accessible, safe, and proven to be more reliable and effective than any other form of “conventional” therapy for recurrent C. difficile infection. Despite its position as a treatment of last resort, FMT has, to the surprise of many, withstood the test of time.10
As one investigator said, “There are few medical therapies that reverse severe illness so dramatically.”23
Author
-

Rebecca J. Anderson holds a bachelor’s in chemistry from Coe College and earned her doctorate in pharmacology from Georgetown University. She has 25 years of experience in pharmaceutical research and development and now works as a technical writer. Her most recent book is Nevirapine and the Quest to End Pediatric AIDS.
View all posts